Tracheostomy and Mechanical Ventilation: Restoring Voice, Swallow, and Upper Aerodigestive Functions
Presented LIVE by Passy Muir
Multidisciplinary – Open to SLPs, RTs, nursing, and any healthcare professional who works with this patient population
Location:
This is a live, virtual course. It will be presented online.
Featuring:
Kristin King, PhD, CCC-SLP; Carmin Bartow, MS, CCC-SLP, BCS-S
Tiffany Oakes, MS, CCC-SLP; Corey Mohnike, BS, RRT; Rachel O’Hare, RRT
In addition to presentation, the seminar includes demonstrations, panel discussions, and case studies
Date:
Saturday, July 23, 2022 9:30am-6:30pm Eastern
Contact hours:
7 LIVE contact hours and up to 5 recorded hours
Overview
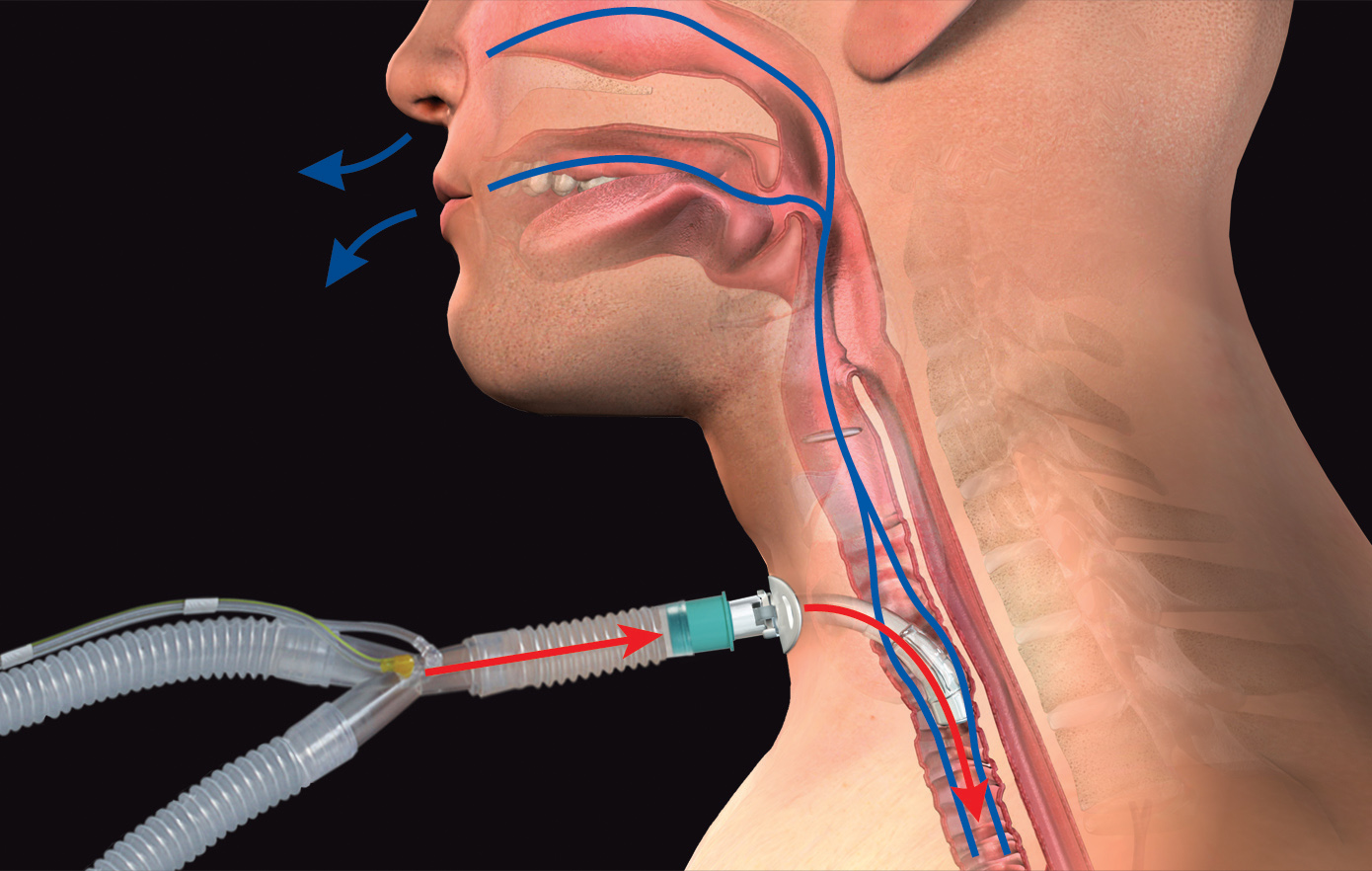
This interactive, virtual seminar reviews the management of patients following tracheostomy and describes the multidisciplinary roles from admission to rehabilitation. It will provide you with the steps and strategies for assessing use of a no-leak speaking Valve when the patient is on mechanical ventilation to transitioning them to Valve use when off the ventilator. Attendees will learn step-by-step methods to evaluate for use of a no-leak speaking valve to restore communication, to improve swallowing and secretion management, and to restore pressures, among other benefits. Both basic and advanced techniques for successful assessment and placement of a no-leak speaking valve in- line with mechanical ventilation will be discussed, including review of ventilator settings and best practice for alarm management. The impact on mobility, infection control, and weaning also will be discussed.
This unique, virtual seminar allows several options to tailor the learning to your experience level. Concurrent sessions for dysphagia, one general and one advanced, and concurrent sessions for ventilator application, one general and one advanced, will be offered. You select the one that fits your level best. All concurrent sessions will be offered as a recorded session for one week following the seminar. Attendees will learn through didactic methods, breakout sessions with interactive learning, patient videos and case studies, and panel discussions.
Speakers

Kristin King, PhD, CCC-SLP
With over 25 years of experience in medical, academic, and industry settings, Dr. King brings a unique perspective to medical speech-language pathology. With a focus on neurological disease processes, her research and teachings have investigated traumatic brain injury, swallowing disorders, and aspects of critical care (tracheostomy and mechanical ventilation). She regularly speaks both domestically and internationally and publishes in peer-reviewed and clinical journals. She also has acted as an expert witness.
Disclosure:
Financial – Dr. King is an employee of Passy Muir Inc.
Nonfinancial – Dr. King has no non-financial disclosures to disclose.

Carmin Bartow, MS, CCC-SLP, BCS-S
Carmin Bartow is a speech-language pathologist who has over 20 years of experience working with medically complex patients in a variety of settings. She is Board Certified in Swallowing and Swallowing Disorders and is a Certified Endoscopist in the state of Tennessee. She has specialized in dysphagia intervention, assessment and treatment of patients with tracheostomy and mechanical ventilation, and in communication and swallowing intervention for patients with head and neck cancer. Carmin was instrumental in the development and success of the Vanderbilt University Medical Center Tracheostomy Team and in the Medical Speech Pathology: Best Practices annual conference. Additionally, she taught the Dysphagia course as an adjunct instructor at Tennessee State University. She has authored and co-authored multiple peer-reviewed papers and presentations on dysphagia, head and neck cancer, tracheostomy and mechanical ventilation, and multidisciplinary tracheostomy teams. Carmin is currently a full-time clinical specialist for Passy Muir.
Disclosure:
Financial – Carmin Bartow is an employee of Passy Muir Inc.
Nonfinancial – Carmin Bartow has no non-financial disclosures to disclose.

Tiffany Oakes, MS, CCC-SLP
Tiffany graduated with a Master’s in Speech-Language Pathology from the University of Tennessee Health Science Center in 2012. She has been a medical SLP in various settings from acute care to home health, treating both the adult and medically complex pediatric populations. Tiffany has experience developing patient care pathways to guide assessment and treatment selection for patients in home health, at both the state and national level. She has participated in research related to patients with TBI and sports concussions, and she has experience with research analysis and writing white papers. She is a volunteer for Remote Area Medical (RAM), assisting with medical services. She also participates in the development of multimedia education related to healthcare and clinical practice.
Disclosure:
Financial – Tiffany Oakes is an employee of Passy Muir Inc.
Nonfinancial – Tiffany Oakes has no non-financial disclosures to disclose.

Corey Mohnike, BS, RRT
Corey Mohnike is a registered respiratory therapist at a Level II Trauma Center. Corey joined the Passy Muir consultant team with significant experience regarding the Passy Muir® Valve. His experience includes use of the Valve both as a patient requiring a tracheostomy after a motor vehicle accident and working with the Valve in medical facilities as an RRT. Corey worked at Madonna Rehabilitation Hospital, a Passy Muir Center of Excellence, in areas that served many ventilator patients using the Valve. He has co-authored multiple procedures regarding Passy Muir Valve assessment and application with patients on mechanical ventilation. Corey served as the Clinical Educator for a multidisciplinary staff at Bryan Health in Lincoln, Nebraska. He was also involved with the Nebraska Society for Respiratory Care, and has spoken at multiple state meetings and national conferences. He is now the RT Educator at The Medical Center of the Rockies in Loveland, CO.
Disclosure:
Financial – Corey Mohnike is an employee of Passy Muir Inc.
Nonfinancial – Corey Mohnike has no non-financial disclosures to disclose.

Rachel O’Hare, RRT
Rachel O’Hare started her respiratory therapy career in the United States Army Reserves where she served 13 years and did one tour in support of Operation Enduring Freedom. After returning home, she began working as a traveler and has worked in hospitals across the United States, including Alaska and Hawaii. She has a very broad knowledge in respiratory care and has worked in all patient care areas, including Adult ICU, Pediatric ICU, and Neonatal ICU. She also has worked in a pulmonary function lab in addition to long-term care. In 2018, Rachel began to pursue her passion of teaching, advancing her career away from the bedside into becoming a clinical educator for critical care ventilation products. She spent the last few years working as a regional clinical educator, providing clinical education and support for all of Northern California before joining the Passy Muir clinical team in 2022.
Disclosure:
Financial – Rachel O’Hare is an employee of Passy Muir Inc.
Nonfinancial – Rachel O’Hare has no non-financial disclosures to disclose.

Kristin Lascano, RRT
Kristin Lascano is a Registered Respiratory Therapist and has varied experiences in respiratory care. Kristin’s background in respiratory therapy started in a NICU and transport of the neonatal patient. Her career continued into the adult acute care setting. Throughout her career, Kristin has assisted with multiple areas of clinical education for multidisciplinary team members, including mock code training, art line insertions, and ABCDE protocols in the ICU. She has also served as a clinical adjunct instructor for the respiratory college in her area. Kristin continues to maintain her clinical skills through PRN work at Baylor Scott & White Health in Texas. She is currently a full-time Clinical Specialist with Passy Muir.
Disclosure:
Financial – Kristin Lascano is an employee of Passy Muir Inc.
Nonfinancial – Kristin Lascano has no non-financial disclosures to disclose.
Agenda
AgendaIf you would like to download a copy of our agenda, click here. |
|
| 9:30 -9:45 am ET | Welcome and review of the agenda/plan for the day |
| 9:45 – 10:45 am ET |
Assessment, Placement, and Troubleshooting – Non-Vent Contact Hours: 60 min Teaching Strategies: Lecture with Q &A Content Area: Clinical Practice Learning outcomes: 1. Discuss the steps to airway patency assessment and Valve placement. 2. List troubleshooting considerations and how to improve patient use. |
| 10:45 – 11:00am ET | Break and transition to sessions |
| 11:00 – 11:30 am ET |
Break Out Session – Cuff Management and Valve Selection Contact Hours: 30 min Teaching Strategies: Demonstrations and Q & A Content Area: Clinical Practice Learning outcomes: 1. List two ways the Valves are the same and different. 2. Demonstrate two methods of proper cuff inflation and deflation techniques. |
| 11:30 – 11:45 am ET | Break and EXPO Q & A |
| 11:45 – 12:45 pm ET |
Concurrent Session One: Patient Assessment and Placement– Basic Ventilator Application Contact Hours: 60 min Teaching Strategies: Lecture with Q & A and case studies Content Area: Clinical Practice Learning outcomes: 1. Discuss patient selection criteria, including airway assessment and ventilator parameters 2. List the steps for successful placement of a no-leak Valve in-line with mechanical ventilation |
| 11:45 -12:45 pm ET | Concurrent Session Two: Ventilator Management and Troubleshooting – Advanced Ventilator Application Contact Hours: 60 min Teaching Strategies: Lecture with Q & A and case studies Content Area: Clinical Practice Learning outcomes: 1. Describe considerations for ventilator management, including PEEP and alarm management 2. Discuss potential issues that require troubleshooting and how to manage them |
| 1:00 – 1:30 pm ET | Break Out Session – Ventilator Application and Q&A Contact Hours: 30 min Teaching Strategies: Demonstration with Q & A Content Area: Clinical Practice Learning outcomes: 1. List two considerations for Valve placement in-line with mechanical ventilation 2. Describe steps to resolving troubleshooting issues. |
| 1:30 – 1:45 pm ET | Break |
| 1:45 – 2:45 pm ET | Ethics and Importance of Teamwork Contact Hours: 60 min Teaching Strategies: Panel discussion with case studies Content Area: Clinical Practice Learning outcomes: 1. Describe two ethical considerations to the evaluation and treatment of patients with tracheostomies 2. List members of a tracheostomy team and the benefits to team management and rounding |
| 2:45 – 3:00 pm ET | Break (networking and Expo) |
| 3:00 – 4:00 pm ET | Concurrent Session Three: Basics of Dysphagia Intervention (for this patient population) Contact Hours: 60 min Teaching Strategies: Lecture with Q &A and case studies Content Area: Clinical Practice Learning outcomes: 1. List assessment and treatment considerations when using a no-leak speaking valve during dysphagia management 2. State the role and importance of upper airway airflow and subglottic pressure for swallowing function |
| 3:00 – 4:00 pm ET | Concurrent Session Four: Advanced Dysphagia Management Contact Hours: 60 min Teaching Strategies: Lecture and Q & A with case studies Content Area: Clinical Practice Learning outcomes: 1. Describe dysphagia assessment considerations with in-line use of the Valve 2. List treatment options and considerations for both in-line mechanical ventilation and non-vent Valve use |
| 5:00 – 6:00 pm ET | Early Intervention, Case Studies, and Troubleshooting Contact Hours: 60 min Teaching Strategies: Panel Discussion with simulations Content Area: Clinical Practice Learning outcomes: 1. List three benefits to early intervention. 2. Identify and provide the solution for two presented scenarios as it relates to troubleshooting with Valve use. |
| 6:00 – 6:30 pm ET | Summary discussion, Q & A, and adjournment |
CEU Information
Continuing education credit offered for RTs, SLPs, and RNs. All others will receive a Certificate of Attendance.

Recorded webinars are offered for .1 ASHA CEUs (intermediate level) each.

Recorded webinars are offered for 1 CRCE each.

Registration / Cost
Space is limited and registrations will be accepted in the order received.
Regular Registration: $199.00
Student Registration: Please contact kking@passymuir.com for information.
Print outs: Handouts will be given on registration and are included in the cost of the course.
Assistance: All participants in Passy-Muir, Inc. Continuing Education Courses are entitled to an accessible, accommodating, and supportive teaching and learning environment. Please inform us of any specific needs so that we may assist you.
Recordings
This seminar offers a unique opportunity to earn additional recorded continuing education credits and to enhance your learning. In preparation for the seminar, we have a one-hour webinar available to provide a foundational review to enhance your experience with the seminar. This pre-requisite webinar will be available starting on July 12th and will remain available through July 22nd.
- PRE-REQUISITE: Fundamentals: From Tracheostomy Tubes to Mechanical Ventilation Terminology (.1 ASHA CEUs; 1 CRCE; 1 contact hour)
Following the seminar, you will have the opportunity to rewatch the concurrent session that you viewed live during the seminar and to take the session that you were not able to view. We will have four one-hour webinars available from July 25th through August 7th. These sessions will provide an opportunity to earn up to an additional four hours of continuing education. These sessions will be:
- Patient Placement and Assessment: Basic Ventilator Application (.1 ASHA CEUs; 1 CRCE; 1 contact hour)
- Ventilator Management and Troubleshooting: Advanced Ventilator Application (.1 ASHA CEUs; 1 CRCE; 1 contact hour)
- Fundamentals of Dysphagia Intervention: Swallowing to the Bedside Assessment and Interventions (.1 ASHA CEUs; 1 CRCE; 1 contact hour)
- Dysphagia Management: From Instrumentals to Considerations with Mechanical Ventilation (.1 ASHA CEUs; 1 CRCE; 1 contact hour)









