Clinician’s Corner features articles on cutting-edge therapies and evidence-based clinical practice drawn from the collaborative efforts of the Passy Muir Clinical Team and expert researchers and clinicians from different disciplines and settings. It is intended to inspire discussion about the Passy Muir® Valve and advancement in issues related to the care and management of patients with tracheostomy and mechanical ventilation.
Impacting Patient Care and Ethical Considerations

Ethical considerations are constantly evolving as medical care changes and advances. Because of the ever-changing state of medical care, being aware of the current research must be maintained at an international level as researchers from around the globe contribute to the standard of care for patients with tracheostomy and mechanical ventilation. However, a challenge to healthcare professionals is clarifying their role in the decision process for medical care and determining appropriate interventions for patients. The ethical standards that should be addressed in practice go beyond individualized, personal professions; they also incorporate the rights of patients and the consideration of a patient’s ability to access communication and to participate in their medical care. The efficiency and efficacy of the communication method provided is a primary aspect to patient care.
Understanding the Management of Patients Undergoing Prolonged Weaning from Mechanical Ventilation

Patients presenting with respiratory failure are now surviving with the help of medical advances, including tracheostomy tubes and mechanical ventilation. The care of patients on mechanical ventilation has changed significantly over recent decades. Since the 1950s, there has been a shift from devices delivering negative-pressure mechanical ventilation to invasive positive pressure ventilation modes. Frequently, ventilation is delivered via tracheostomy tubes and permits prolonged mechanical respiratory support for most individuals with respiratory failure. The presence of the tracheostomy tube accomplishes multiple airway management goals; establishing a patent airway, as well as providing a connection to assisted ventilation.
Tracheostomy Tube Cuff: Purpose and Practice through Team Management

Care of patients with tracheostomy has become a frequent topic of discussion in the medical industry and publications. Due to this focus, details related to the care plan of such patients are of concern and must be considered. This brief discussion highlights one aspect of patient care which has been noted to be of importance, the safety and efficacy of cuff deflation, especially when using a bias-closed position, no-leak Valve.
Case Study: Management of Complications Following SCI and the Role of SLPs on a Multidisciplinary Team

On a splendid, early summer’s day in June 2016, Mr. Walter had the urge to get on his mountain bike after having dinner with his wife and four school-age children. Like every evening, Mr. Walter promised to tell a bedtime story to the two younger children when he returned. So, they waited excitedly for the made-up adventures of the heroes, which Mr. Walter created from his imagination. Mr. Walter was an avid biker and, despite being almost 50 years old, he was in exceptionally good physical condition. He loved being physically active on weekends or after a stressful day at work, breathing fresh air on forest trails, disconnecting for a while, and recharging his batteries through bike riding. Biking was his passion.
High Flow Oxygen Therapy and the PMV®

A frequent question that has arisen from clinicians is: What is High Flow Oxygen Therapy, and should I be using it with my patients who have a Passy Muir® Valve (PMV®)? This article begins to address the considerations by providing information on both devices and the current state of the science. First, High Flow Oxygen Therapy (HFOT) is an oxygen delivery system which provides heated humidity with high flow levels of oxygen (O2). Traditional oxygen delivery systems do not exceed 16 L/min while HFOT can deliver up to 60 L/min and as high as 100% oxygen (Lindenauer, et al., 2014; Gotera, Díaz Lobato, Pinto, & Winck, 2013). HFOT is typically used with patients following acute respiratory failure; however, it has proven to be successful in decreasing the Work of Breathing (WOB) in chronic conditions, such as Chronic Obstructive Pulmonary Disease (COPD) and end-stage cancers as well (Gotera et al., 2013).
Articles Representing International Research on Tracheostomy, Mechanical Ventilation and Passy Muir® Valves

It has been reported by patients that the inability to communicate effectively with healthcare professionals has led to misunderstandings as to their needs, causing increased administration of pain medications and other factors negatively impacting their care. Kinneally reports that use of a tracheostomy tube, instead of an endotracheal tube, enables less use of sedation. This article reports that early use of speaking valves (SV) has become common practice in his ICU. By using SVs earlier during patient care in the ICU, Kinneally reports that the return of verbal communication has been observed to improve patient care and has increased patient and family engagement. He also describes how this appears to be associated with reduced agitation. Because of these changes in patient access to communication, Kinneally reports that the use of sedatives and pain medications has been reduced significantly. Overall, less sedatives are being used when patients have access to their voice, communication, and interaction in their care. These findings suggest that early intervention of SV use with patients in the ICU will improve overall care by reducing the need for pain and sedating medications.
Having a Protocol for Clinical and Research Use of the Passy Muir® Speaking Valve

St. Mary’s Healthcare System for Children is an organization that provides intensive rehabilitation, specialized care, post-acute care, and education for children with life-limiting and medically complex conditions. Established more than 140 years ago, St. Mary’s Hospital for Children is a 97-bed inpatient facility, located in Queens, New York. With a family centered approach, this facility provides medical daycare to children and young adults. It also provides early education for medical conditions, a multidisciplinary feeding disorder program, and a K-12 public school, which provides ongoing education to its long-term inpatients who may be admitted for several months or even years. The feeding program is designed for both inpatient and outpatient cases. Additionally, the hospital’s home care program reaches nearly 2,000 medically fragile children each day throughout New York City and Long Island, making St. Mary’s Hospital for Children one of the largest providers of long term home healthcare for children in the state of New York.
Assessment Considerations for PMV® Candidacy in the Pediatric Population

Premature birth is defined as birth before 37 weeks gestation and is the leading cause of death in babies in the United States. According to the March of Dimes, for the first time in eight years, the preterm birth rate in the United States has increased to 9.63% as reported by the National Center for Health Statistics (NCHS) (2016 Premature Birth Report Card, 2016). These premature infants often face health issues such as respiratory complications, jaundice, retinopathy of prematurity, developmental delays, and gastrointestinal complications, among others. The National Academy of Medicine reports that preterm birth costs $26 billion dollars annually. Due to advances in medical technology and scientific innovation, more micro-preemies, those born at less than 26 weeks gestation or less than 800g, and those with congenital abnormalities are surviving, but not without frequently facing prolonged medical challenges.
Candidacy for Passy Muir® Valve Placement in Infants and Young Children: The Airway Assessment

Assessment of the upper airway is a critical component for a comprehensive evaluation of any infant or very young child who has a tracheostomy. It is the analysis and interpretation of the data collected during the airway assessment that guides the decision-making regarding two critical quality of life issues for very young patients with tracheostomies and their families: (1) the route for nutritional intake and (2) candidacy for Passy Muir® Valve placement and wear time. Use of the Passy Muir Valve not only addresses neurodevelopment but also health-related quality of life.
Keys to Success: A Pediatric Respiratory Therapy Case Study

Throughout infancy and childhood, gross and fine motor development progresses in a typical pattern and timeline which impacts many aspects of a child’s life. However, when infants and children are tracheostomized at a young age, this developmental process is negatively impacted. Placement of a tracheostomy tube in the child’s airway opens a previously closed system. While the tracheostomy is necessary to improve the respiratory status of the child, having a tracheostomy tube in place changes the dynamics of the aerodigestive system. The child now breathes through the tracheostomy tube and cannot use the upper airway effectively, especially if the tracheostomy tube cuff is inflated. This loss of airflow through the upper airway diminishes stimulation of the upper airway, causing changes in sensation, loss of subglottic pressure, negative impact on secretions and secretion management, changes in swallow function, loss of voicing, and other negative changes to functions. In addition, having an open system has been shown to have a negative effect on trunk support and core stability for mobility (Massery, 2014, 2006; Massery, Hagins, Stafford, Moerchen, & Hodges, 2013). It also reduces their ability to communicate and eat safely. Early intervention is imperative, as a disruption during this critical period may have significant impact on patients’ development, in particular to language and speech (Stevens, Finch, Justice, & Geiger, 2011). The sooner the clinical team is able to intervene, the risk for long term delays is decreased (Hofmann, Bolton, & Ferry, 2008).
Physicians’ Perspective on the Passy Muir® Speaking Valve

Barlow Respiratory Hospital is a unique place to practice medicine. The hospital is small, only 60 beds on the main campus in Los Angeles. The hospital was founded in 1902 as a Tuberculosis Sanatorium and remains surrounded by nature, despite its location only a few miles from downtown. At Barlow Respiratory Hospital, our interdisciplinary staff is tight-knit and works as a team. Our patients are primarily transferred to us from intensive care units at other facilities in the surrounding area. We have developed an effective methodology for in-line use of the Passy Muir® Valve with mechanically ventilated patients.
Evidence Based Support for Using a PMV® In-line with Mechanical Ventilation

Misconceptions exist about potential risks for harming a patient’s already-compromised lungs during recovery if a speaking valve is used with patients who are mechanically ventilated, and these misconceptions tend to hinder use of speaking valves with this population. Arguments about use of a one way speaking valve during mechanical ventilation include the ideas that there are increased risks of aspiration due to cuff deflation, decreased lung recruitment because of lost ventilation with cuff deflation, and even increased risk of barotrauma because of increased lung pressures. While the purpose of mechanical ventilation is to support the respiratory system during recovery, the changes it causes in the physiologic function of the respiratory system also lead to deleterious effects on secretion management, lung function, communication, swallowing, subglottic pressure, and other parameters affecting function. Frequently, the potential risks are used as reasons to delay use of a speaking valve in-line on the ventilator; however, research does not support them. These a priori assumptions are not substantiated with research, and clinical observations have been providing anecdotal evidence that was contrary to prior teachings. Previously, there has been a paucity of research to support what has been seen clinically; however, current empirical research is demonstrating that the use of a speaking valve in-line with mechanical ventilation is promoting improved ventilation (Sutt et al., 2016) and faster weaning (Carmona et al., 2015), among other benefits.
Effects of PMV® In-line with Mechanical Ventilation on Communication and Swallowing

Annually, more than 100,000 patients in the United States experience medical events that require a tracheostomy, with 24 percent of those necessitating mechanical ventilation (Yu, 2010). It is estimated that by the year 2020, there will be over 600,000 patients requiring prolonged mechanical ventilation (Zilberberg, 2008). Most vented patients are on prolonged bedrest during hospitalization. In intensive care units across the country, efforts are being made to implement early mobility programs as there is significant evidence indicating that many patients in intensive care units on prolonged mechanical ventilation experience a marked decline in functional status (Spicher, 1987). After one week of bedrest, muscle strength may decrease by as much as 20 percent with an additional loss of 20 percent each subsequent week of bedrest (Perme, 2009; Sciaky, 1994). Why is this significant to speech-language pathology?
Speaking Valve Use During Mechanical Ventilation: More than Just for Communication and Swallowing

The inability to communicate during periods of mechanical ventilation (MV) can increase psychoemotional distress (Egbers, Bultsma, Middlekamp, & Beoerma, 2014) and has been associated with depression and post-traumatic stress disorder (Freeman -Sanderson, Togher, Elkins & Phipps, 2016). One way speaking valves can be used to restore verbal communication for patients who require MV. The Passy Muir® Valve is the only bias-closed position valve that can be used during MV. The Passy Muir Valve opens during inspiration and closes at the end of inspiration, re-directing exhalation through the vocal cords and out through the mouth and nose, which allows for verbal communication. The restoration of airflow, sensation, and positive airway pressure to the aerodigestive tract returns the upper airway to a more normal physiologic condition and may also have other clinical benefits for the patient who requires tracheostomy and MV.
Current Research Related to Mechanical Ventilation and Speaking Valve Use

Current research shows an overwhelming association of negative emotions, including fear, anxiety and depression with patients admitted to the intensive care unit (ICU). Statistics report up to 75% of patients report anxiety and 40% report depressive symptoms following admission to ICU (Nelson et al. 2001). These investigators conducted a prospective, observational study of 22 patients in a tertiary ICU, to evaluate the effects of vocal communication on mental and physical wellness. The study measured patient-reported change of mood, communication-related quality of life, and general health status with return of voice among mechanically ventilated tracheostomy patients admitted to the ICU. Daily evaluations were conducted to assess patients’ quality of life in relation to communication, and weekly evaluations were conducted to assess their general health status. All participants had undergone a tracheostomy and experienced voicelessness during mechanical ventilation. Patients progressed through cuff deflation, assessment/management of swallowing, and a communication assessment, which included implementation of the Passy Muir® speaking valve.
Infants and Children with Tracheostomy and Ventilator Dependence in the Intensive Care Units: Candidacy and Early Intervention with a Bias-Closed, No-Leak Speaking Valve

Extensive research on the Passy Muir® Tracheostomy & Ventilator Swallowing and Speaking Valve (PMV®) exists within the adult population to support the benefits of voicing, secretion management, physiologic PEEP, swallowing, olfaction, quality of life, and weaning. However, working with infants and children, who have tracheostomies with or without ventilator support, can be more challenging than with adults due to multiple factors. Developmental factors, in combination with medical concerns, impact treatment considerations, but the research literature in the pediatric population is inadequate to provide sufficient evidence-based practices (Suiter, McCullough & Powell, 2003). Review of recent literature suggests that approximately half of all pediatric patients who receive a tracheostomy are younger than one year of age (Barbato, Bottecchia & Snijders, 2012; Lewis, Carron, Perkins, Sie & Feudtner, 2003). Early tracheostomy may lead to an opportunity for early application of the PMV that may otherwise be missed if the medical team does not have a clear understanding of practice guidelines for PMV application.
From ICU to Home Care: A Protocol for Transitioning

The Tracheostomy and Home Ventilator Program at Children’s Hospital of Wisconsin is primarily comprised of children with a history of prematurity, severe bronchopulmonary dysplasia, and airway abnormalities. The care team includes neonatal and pediatric intensivists, pulmonologists and otolaryngologists, along with other consulting services. Additionally, the child is followed by the Trach/Vent Team comprised of RN (registered nurse) care coordinators, respiratory therapists, social workers, and discharge planners. The team meets weekly with the family and bedside nursing staff to outline progress towards discharge.
Delivering Complex Care for Complex Children: A Multidisciplinary Approach

An increasingly visible trend exists regarding efforts to improve the care of children with complex aerodigestive disorders. For many years and a variety of reasons, children with complex disorders have often been cared for in tertiary referral centers. Such centers have provided the availability of a wide range of subspecialty care. Multidisciplinary care centers have existed for many years to treat children with craniofacial anomalies, cystic fibrosis, and cancer. However, recently, pediatric aerodigestive centers have had increasing visibility and marketing presence. As such, it is important to understand who is involved, why such centers exist, and what it means.
Protocols Assist with Improving Communication for Patients with Tracheostomy & Ventilator Dependence

For patients with tracheostomy and ventilator dependence, communication in the intensive care unit can be difficult to achieve but having a reliable means of communication is imperative for health, safety, and well-being. The Speech-Language Pathology (SLP) team at Vanderbilt University Medical Center (VUMC) recently launched a six-month quality improvement initiative to promote early intervention for this patient population. The project, “Improving Communication for Patients with Tracheostomy and Ventilator Dependence,” had a primary goal of establishing consistency with communication for these patients by having the entire SLP department trained in a newly developed protocol. Prior to this project, only some of the SLPs in the department were fully confident and competent in providing intervention to these patients. With the development and implementation of this program, patients may participate more readily in their medical plan, which can improve efficiency of care by all staff, preventing unnecessary delays in their care, which may have occurred secondary to the earlier difficulties with communication and patient participation.
Having Protocols for Clinical Use to Improve Patient Outcomes

Gaylord Specialty Healthcare was founded in 1902 as a tuberculosis sanatorium and has grown into a 137-bed long-term acute care hospital (LTACH) facility. Within this facility, specialties focus on the medical management and rehabilitation of patients who have suffered acute illness or a traumatic accident. Because of this focus, programs have been established in Pulmonary, Spinal Cord Injury, Traumatic Brain Injury, and Stroke as major diagnostic areas to provide intervention. Care of these medically complex patients is provided by a multidisciplinary team, including physicians, nurse specialists, respiratory care practitioners, radiology technicians, therapists (physical, occupational, and speech-language pathology), pharmacists, and care managers, for both adolescents and adults. The medically complex populations being seen also may include those patients with chronic obstructive pulmonary disease (COPD), restrictive lung disease, chronic emphysema, obstructive sleep apnea, bronchitis, asthma, respiratory complications from morbid obesity, and neurological disorders. Additionally, complex diagnoses also include muscular dystrophy and post-polio syndrome, as well as ventilator dependence due to illness or injury. Because of the wide range and complexity of the diagnoses being treated, a multidisciplinary team is essential to provide best outcomes.
Using the Passy Muir® Valve in Conjunction with High Flow Oxygen Therapy

Our facility, Madonna Rehabilitation Hospitals, utilizes warm mist humidification during the care of patients with tracheostomy. As innovation is one of the facility’s core values, the Vapotherm Precision Flow device for High Flow Oxygen Therapy (HFOT) was introduced at Madonna in January 2016. This technology allows for delivery of gas flow rates of up to 40 LPM (liters per minute) without discomfort or damage to airway epithelia (Lindenauer, Stefan, Shieh, Pekow, Rothberg, & Hill, 2014).
The Role of Pressures in Swallowing and Impact of the Passy Muir® Valve

The presence of a tracheostomy tube has been associated with aspiration and dysphagia, but exact prevalence has varied in the literature. Tracheostomy tubes have been shown to limit laryngeal elevation, decrease subglottic pressure, and mechanically alter the swallow (Suiter, McCullough, & Powell, 2003). Patients with tracheostomy tubes also have other risk factors, aside from the presence of the tracheostomy tube, that may predispose them to aspiration or dysphagia. This article will discuss the role of subglottic pressure and its relation to swallowing.
Clinical Relevance of the Sensorimotor Pathways in Dysphagia Management following Tracheostomy
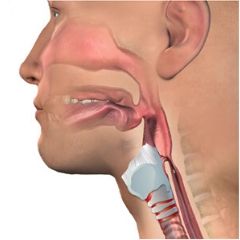
The oropharyngeal and esophageal swallowing systems are a challenge to understand fully due to the interdependence of sensory, motor, and behavioral systems. When patients are tracheostomy-dependent, assessment of their swallowing, establishment of the least restrictive diet, and identification of interventions to improve swallowing function pose a more difficult challenge than with patients who have an intact system. Airway protection in these patients becomes highly dependent on reintegration of the upper aerodigestive tract, use of compensatory abilities, medical status, and the integrity of the physiologic aspects of swallowing. An understanding of these systems is an essential precursor to appreciating how they interplay and relate to swallowing safety in patients with tracheostomies.














