This is a resource for people who would like to learn more about tracheostomies.
What is a Tracheostomy Tube?
When a tracheotomy procedure is performed, a hole is made in the trachea (windpipe), and a tracheostomy tube is inserted. This tube provides an artificial airway for the patient.
Parts of a Tracheostomy Tube
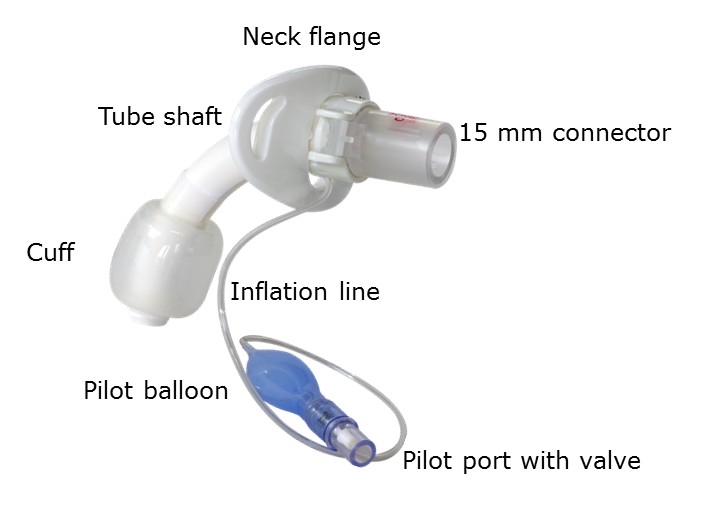
Tracheostomy tubes vary by manufacturer and by type. For example, there are neo-natal, pediatric, and adult tracheostomy tubes, and some tubes have cuffs, while others do not. The diagram below shows the basic parts of a tracheostomy tube.
 Tracheostomy Equipment
Tracheostomy Equipment
In a home setting, a caregiver should have enough equipment to perform suction, skin care, tracheostomy tube changes, and possibly humidification. In a hospital setting, it is important that these materials are within reach of the staff caring for the tracheostomized individual.
 Stoma Care
Stoma Care
Care of the tracheostomy stoma is an important part of daily tracheostomy care. The build up of mucus and rubbing of the tracheostomy tube can cause irritation and infection. The skin around the stoma should be cleaned at least twice a day to help prevent these problems. If the area around the stoma appears irritated, is tender or has a bad odor the stoma should be cleaned more often.
Changing the tracheostomy tube is typically a two-person procedure. The clinician who removes the tracheostomy tube should be the individual to insert the new tube to allow for assessment of the patient’s airway for any anomalies or resistance. Before beginning the procedure, insure that all equipment for the tracheostomy tube change is at the patient’s bedside. Inspect the new tracheostomy tube for any signs of damage and make sure all the equipment is functional. Insertion of a tracheostomy tube with a smaller outer diameter is generally easier than changing to a larger tube. The tracheostomy tube change should occur before a meal, or at least one hour after a meal to minimize the risk of aspiration.
 Secretion Management
Secretion Management
Normally, the upper airway functions to warm, filter, and humidify the air. Secretions are managed by mucociliary transport (a process that occurs in the airway to move material upwards and away from the lungs), swallowing secretions, or by coughing and expectorating the secretions through the oral cavity. These natural mechanisms are impaired with a tracheostomy tube, due to the bypassing of the upper airway. This can lead to secretion retention which can cause increased airway resistance and increased work of breathing. Therefore, mobilization of secretions is one of the most important aspects of tracheostomy care. Clearing the airway is an important mechanism for secretion management which is performed through coughing or suctioning. Proper humidification, systematic hydration, and mobilization are also crucial for secretion mobilization.
 Humidity
Humidity
Humidification is a crucial part of tracheostomy care, across the continuum of care. Humidification is necessary because the normal humidification and filtration system is bypassed with the tracheostomy tube. Therefore air inspired by the patient with a tracheostomy will be cold and dry.
Humification should be part of the patient’s care if the patient is using mechanical ventilation or if the patient has thick secretions (Mitchell, 2013).
Cool and heated systems
Heated humidifiers work by increasing the heat and water vapour content of inspired gas.
 Heat-Moisture Exchanger (HME)
Heat-Moisture Exchanger (HME)
HMEs retain heat and moisture of the patient’s expired air to warm and humidified the next inspired breath.
NOTE: An HME will be ineffective when a speaking valve is in place. This is due to the fact that, while wearing a speaking valve, the exhaled air does not exit through the tracheostomy tube and HME, but through the nose and mouth.
 Monitoring Devices
Monitoring Devices
Proper patient monitoring is essential in the management of the patient with tracheostomy. Common monitoring devices include arterial blood gases, pulse oximetry, capnography, and spirometry.
Pulse Oximetry:
Pulse oximetry has become the standard of care for monitoring patients throughout the continuum of care. It is used to determine the oxygen saturation of arterial hemoglobin, or the ability of the blood to transport oxygen throughout the body.
In addition to oxygen saturation, many pulse oximeters also display heart rate.
To learn more, please contact us.










