Using the Passy Muir® Valve in Conjunction with High Flow Oxygen Therapy
Melissa Gulizia, BS, RRT | Cheryl Wagoner, MS, CCC-SLP, BCS-S

Our facility, Madonna Rehabilitation Hospitals, utilizes warm mist humidification during the care of patients with tracheostomy. As innovation is one of the facility’s core values, the Vapotherm Precision Flow device for High Flow Oxygen Therapy (HFOT) was introduced at Madonna in January 2016. This technology allows for delivery of gas flow rates of up to 40 LPM (liters per minute) without discomfort or damage to airway epithelia (Lindenauer, Stefan, Shieh, Pekow, Rothberg, & Hill, 2014). Key clinical benefits of the Vapotherm Precision Flow device include:
- Humidification at body temperature and saturated – 37°C.
- Delivering consistent, energetically stable, vapor phase humidity.
- Rainout prevention.
- Mitigation of contamination via humidity.
- Mitigation of stoma irritation.
- Better secretion mobilization.
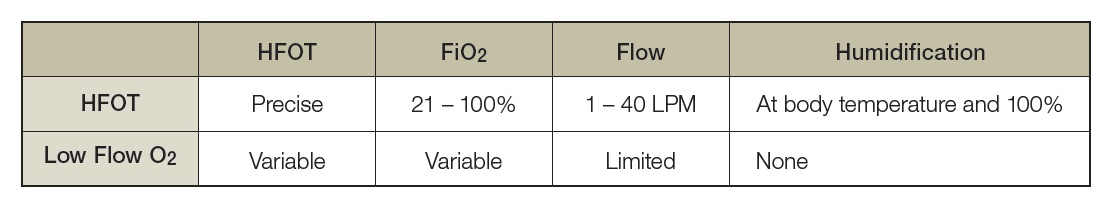
A comparison of HFOT and low flow O2 (oxygen) demonstrates that:
In January 2016, HFOT was used consistently in the Specialty or LTACH units, including patients with tracheostomy tubes. In 2017, Madonna Rehabilitation Hospitals earned recognition as the second Vapotherm Center of Excellence in the United States. A year later, HFOT use was expanded to include the Acute Rehabilitation and Pediatric Hospitals. Currently, use of Vapotherm has been extended to include the longterm ventilator assist unit and the Skilled Nursing Facility level of care. Facility protocols for ventilator weaning and tracheostomy decannulation processes were updated to standardize the safe application of HFOT. In addition, multidisciplinary competencies were developed for staff training that provide for:
- Indications, contraindications, risks, and guidelines.
- Patient safety.
- Application of HFOT.
- Procedures for safety and use.
Indications for Use
HFOT is indicated for patients requiring:
- Humidification of an airway stoma, with or without a tracheostomy tube or larynx tube.
- High oxygen needs.
- A need for high flow therapy.
Patient selection also includes those patients exhibiting increased work of breathing or refractory hypoxemia (generally refers to inadequate arterial oxygenation despite optimal levels of inspired oxygen or onset of barotrauma in mechanically ventilated patients).
Patient Safety and Application
Tracheostomy Tube Application: Connect a patient to HFOT using a 22mm tubing adapter to their tracheostomy mask or T-piece. Do NOT connect the delivery tubing or the tubing adapter directly to a patient’s tracheostomy tube. The tracheostomy tube cuff must be completely deflated when using the Passy Muir® Valve (PMV®), including in conjunction with HFOT. If the Passy Muir Valve is not being used, the tracheostomy cuff may remain either inflated or deflated, as needed for the patient.
Nasal Cannula Application: Nasal cannula application may be used during the tracheostomy tube weaning process, when the tracheostomy tube is capped, or with use of the PMV. The nasal cannula application is then utilized for humidifying the upper airway to help jumpstart the natural system and ensure success with secretion mobilization and tracheostomy tube weaning. The flow that is given by the nasal cannula application also helps to flush out the upper airway or deadspace of CO2; decreases work of breathing; and overall, increases patient comfort and satisfaction.
Outcomes
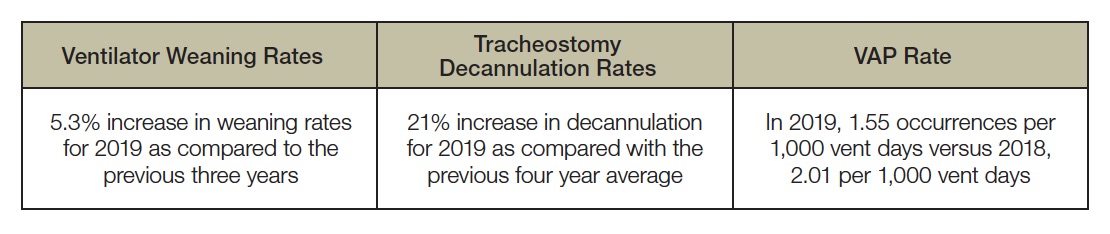
Over the last three years of utilizing the Vapotherm, positive outcomes in numerous areas have been observed. Not only have objective changes in care measurements been observed, but patients’ anecdotal reports include reports of improvement in comfort, noise, and overall, satisfaction. Staff also reports that HFOT has allowed efficiency of care and participation in therapy, including early mobilization. It also allows the staff to focus on other important patient care needs. Lastly, since the Passy Muir Valve can be used in conjunction with HFOT, communication for the patient is improved and increases their participation in their medical care decisions.
Use of HFOT and the PMV have led to the following changes in quality improvements for patients:
Case Study
Karen, a 74-year-old female, was admitted post-emergent left ventricular assist device (LVAD) placement due to a mixed cardiomyopathy that was related to coronary artery disease and chemotherapy for breast cancer. Her acute care stay was complicated by renal failure, requiring hemodialysis; right ventricular heart failure; and respiratory failure, requiring mechanical ventilation and tracheostomy tube.
Upon arrival, Karen was ventilator dependent 24 hours per day. She required a multidisciplinary team approach to establish an individualized plan of care. This multidisciplinary team consisted of physicians, respiratory therapists, speech-language pathologists, physical and occupational therapists, nutritionist, nursing staff, and others. The initial plan of care included primary goals to address mobility, self-care, ventilator/tracheostomy tube weaning, and dysphagia.

Despite Karen’s complex medical history, integrating rehabilitation with medical management would contribute to optimal outcomes. Management included the use of protocols for ventilator weaning and tracheostomy tube weaning. These protocols are typically instituted upon admission as part of the admission order sets and the standard of care. With these protocols, both use of the Passy Muir Valve and HFOT were implemented to improve communication and humidification for the patient. Each healthcare discipline provided a different focus for therapy. The comprehensive plan of care included mobility, communication, dysphagia, self-care, and respiratory management.
Upon admission, Karen was evaluated for mobility, self-care, and swallowing function. Evaluation results indicated that Karen’s functional levels upon admission were:
- Maximum Assistance for mobility, transfers, and dressing.
- Minimum Assistance for grooming and eating.
- Severe dysphagia with a determination for nil per os (NPO or nothing by mouth).
At the time of admission, Karen also was ventilator dependent and her ventilator settings were:
- Ventilator Settings without the Passy Muir Valve
- PC/AC (Pressure Control/Assist Control) o Vt (Tidal Volume) = ~500
- PC (Pressure Control) = 17 cmH2O
- PEEP (Positive End-Expiratory Pressure) = 7 cmH2O
- RR (Respiratory Rate) = 12 bpm (breaths per minute)
- FiO2 of 35%
- Ventilator Settings with the Passy Muir Valve o NIV S/T (Non-Invasive Ventilation, Spontaneous Timed
- Vt = ~500
- PC = 28 cmH2O
- PEEP = 0 cmH2O
- RR = 12 bpm
- FiO2 of 30%
She also was provided with HFOT and the settings for the Vapotherm with the Passy Muir Valve in place were a flow of 20 – 25 LPM, temperature of 37° C, and an FiO2 of 30%-40%.
Due to Karen’s complex medical needs, ongoing assessment and collaboration with the team were necessary throughout her stay. This integrated, multidisciplinary approach ensured that Karen’s respiratory needs were met in a safe and effective manner.
With both the input of the multidisciplinary team and the implementation of the appropriate protocols, Karen progressed to the following functional levels:
- Standby assistance for walking and bathing.
- Minimum Assistance for dressing; however, her limitations were due to the LVAD and edema.
- Returning to a regular diet without restrictions for food consistency or diet levels. She had a regular diet with thin liquids.
Karen was successfully weaned off the ventilator during her stay. She also progressed to decannulation, having her tracheostomy tube removed. The current plan is for her to return home soon. Prior to her discharge home, Karen and her husband will go on a community outing to practice skills and ensure safety.
Conclusion
Implementing standard protocols and having a multidisciplinary team providing a plan of care has been shown to improve patient outcomes (Santos, Harper, Gandy, & Buchanan, 2018). Using both HFOT and a standard decannulation protocol (see the Decannulation Protocol on page 29), patients, such as Karen, may progress to higher levels of function and independence (Gotera, Díaz Lobato, Pinto, & Winck, 2013). A patient with a tracheostomy tube and mechanical ventilation has implications for all clinical professions and each clinician is essential to the plan of care. The use of HFOT has been shown to enhance secretion management and facilitate weaning. It is through the use of standard protocols for HFOT and the PMV in tracheostomy care that facilities have found faster weaning times, which decreases overall lengths of stay and medical costs.
This article is from the Fall 2019 Protocol Issue of Aerodigestive Health. Click here to view Using the Passy Muir® Valve in Conjunction with High Flow Oxygen Therapy.
References
Lindenauer, P. K., Stefan, M. S., Shieh, M. S., Pekow, P. S., Rothberg, M. B., & Hill, N. S. (2014). Outcomes associated with invasive and noninvasive ventilation among patients hospitalized with exacerbations of chronic obstructive pulmonary disease. JAMA Internal Medicine, 174(12),1982-93.
Gotera, C., Díaz Lobato, S., Pinto, T., & Winck, J. C. (2013). Clinical evidence on high-flow oxygen therapy and active humidification in adults. Pulmonology Journal (Revista Portuguesta de Pneumologia), 19 (5), 217-227.
Santos, A., Harper, D., Gandy, S., & Buchanan, B. (2018). 1214: The positive impact of multidisciplinary tracheostomy team in the care of post-tracheostomy patients. Critical Care Medicine, 46 (1), 591.doi: 10.1097/01.ccm.0000529218.20247.15












